Carotid Artery Disease
Vascular surgeons at UCSF have over five decades of proven experience in preventing strokes with carotid artery surgery, and in treating rare disorders of the carotid arteries such as fibromuscular dysplasia. The UCSF Vascular Surgery Program has also earned the highest designation for quality outcomes in carotid artery surgery by the Leapfrog Initiative, that compared outcomes in carotid artery surgeries throughout Northern California.
Carotid artery disease is a disease in which a waxy substance called plaque builds up inside the carotid arteries.
You have two common carotid arteries, one on each side of your neck, that each divide into internal and external carotid arteries. The internal carotid arteries supply oxygen-rich blood to your brain, while the external carotid arteries supply oxygen-rich blood to your face, scalp, and neck.
Carotid Arteries
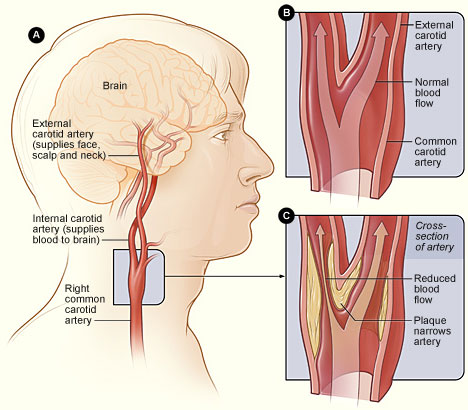
Figure A shows the location of the right carotid artery in the head and neck. Figure B shows the inside of a normal carotid artery that has normal blood flow. Figure C shows the inside of a carotid artery that has plaque buildup and reduced blood flow.
Carotid artery disease is serious because it can cause a stroke, also called a “brain attack.” A stroke occurs if blood flow to your brain is cut off.
If blood flow is cut off for more than a few minutes, the cells in your brain start to die. This impairs the parts of the body that the brain cells control. A stroke can cause:
- Lasting brain damage,
- Long-term disability, such as vision or speech problems or paralysis (an inability to move),
- Or death.
Overview
Carotid artery disease is a major cause of stroke in the United States. Over time, plaque hardens and narrows the arteries. This may limit the flow of oxygen-rich blood to your organs and other parts of your body.
Atherosclerosis can affect any artery in the body. For example, if plaque builds up in the coronary (heart) arteries, a heart attack can occur. If plaque builds up in the carotid arteries, a stroke can occur.
What Causes Carotid Artery Disease?
Carotid artery disease seems to start when damage occurs to the inner layers of the carotid arteries. Major factors that contribute to damage include:
- Smoking
- High levels of certain fats and cholesterol in the blood
- High blood pressure
- High levels of sugar in the blood due to insulin resistance or diabetes
When damage occurs, your body starts a healing process. The healing may cause plaque to build up where the arteries are damaged.
The plaque in an artery can crack or rupture. If this happens, blood cell fragments called platelets will stick to the site of the injury and may clump together to form blood clots.
The buildup of plaque or blood clots can severely narrow or block the carotid arteries. This limits the flow of oxygen-rich blood to your brain, which can cause a stroke.
Who Is at Risk for Carotid Artery Disease?
The major risk factors for carotid artery disease, listed below, also are the major risk factors for coronary heart disease (also called coronary artery disease) and peripheral artery disease (P.A.D.).
- Diabetes. With this disease, the body’s blood sugar level is too high because the body doesn’t make enough insulin or doesn’t use its insulin properly. People who have diabetes are four times more likely to have carotid artery disease than people who don’t have diabetes.
- Family history of atherosclerosis. People who have a family history of atherosclerosis are more likely to develop carotid artery disease.
- High blood pressure (Hypertension). Blood pressure is considered high if it stays at or above 140/90 mmHg over time. If you have diabetes or chronic kidney disease, high blood pressure is defined as 130/80 mmHg or higher. (The mmHg is millimeters of mercury—the units used to measure blood pressure.)
- Lack of physical activity. Too much sitting (sedentary lifestyle) and a lack of aerobic activity can worsen other risk factors for carotid artery disease, such as unhealthy blood cholesterol levels, high blood pressure, diabetes, and overweight or obesity.
- Metabolic syndrome. Metabolic syndrome is the name for a group of risk factors that raise your risk for stroke and other health problems, such as diabetes and heart disease. The five metabolic risk factors are a large waistline (abdominal obesity), a high triglyceride level (a type of fat found in the blood), a low HDL cholesterol level, high blood pressure, and high blood sugar. Metabolic syndrome is diagnosed if you have at least three of these metabolic risk factors.
- Older age. As you age, your risk for atherosclerosis increases. The process of atherosclerosis begins in youth and typically progresses over many decades before diseases develop.
- Overweight or obesity. The terms “overweight” and “obesity” refer to body weight that’s greater than what is considered healthy for a certain height.
- Smoking. Smoking can damage and tighten blood vessels, lead to unhealthy cholesterol levels, and raise blood pressure. Smoking also can limit how much oxygen reaches the body’s tissues.
- Unhealthy blood cholesterol levels. This includes high LDL (“bad”) cholesterol) and low HDL (“good”) cholesterol.
- Unhealthy diet. An unhealthy diet can raise your risk for carotid artery disease. Foods that are high in saturated and transfats, cholesterol, sodium, and sugar can worsen other risk factors for carotid artery disease.
Having any of these risk factors does not guarantee that you’ll develop carotid artery disease. However, if you know that you have one or more risk factors, you can take steps to help prevent or delay the disease.
If you have plaque buildup in your carotid arteries, you also may have plaque buildup in other arteries. People who have carotid artery disease also are at increased risk for coronary heart disease.
What Are the Signs and Symptoms of Carotid Artery Disease?
Carotid artery disease may not cause signs or symptoms until it severely narrows or blocks a carotid artery. Signs and symptoms may include a bruit, a transient ischemic attack (TIA), or a stroke.
Bruit
During a physical exam, your doctor may listen to your carotid arteries with a stethoscope. He or she may hear a whooshing sound called a bruit. This sound may suggest changed or reduced blood flow due to plaque buildup. To find out more, your doctor may recommend tests.
Not all people who have carotid artery disease have bruits.
Transient Ischemic Attack (Mini-Stroke)
For some people, having a transient ischemic attack (TIA), or “mini-stroke,” is the first sign of carotid artery disease. During a mini-stroke, you may have some or all of the symptoms of a stroke. However, the symptoms usually go away on their own within 24 hours.
Stroke and mini-stroke symptoms may include:
- A sudden, severe headache with no known cause
- Dizziness or loss of balance
- Inability to move one or more of your limbs
- Sudden trouble seeing in one or both eyes
- Sudden weakness or numbness in the face or limbs, often on just one side of the body
- Trouble speaking or understanding speech
Even if the symptoms stop quickly, call 9–1–1 for emergency help. Do not drive yourself to the hospital. It’s important to get checked and to get treatment started as soon as possible.
A mini-stroke is a warning sign that you’re at high risk of having a stroke. You shouldn’t ignore these symptoms. Getting medical care can help find possible causes of a mini-stroke and help you manage risk factors. These actions might prevent a future stroke.
Although a mini-stroke may warn of a stroke, it doesn’t predict when a stroke will happen. A stroke may occur days, weeks, or even months after a mini-stroke.
Stroke
The symptoms of a stroke are the same as those of a mini-stroke, but the results are not. A stroke can cause lasting brain damage; long-term disability, such as vision or speech problems or paralysis (an inability to move); or death. Most people who have strokes have not previously had warning mini-strokes.
Getting treatment for a stroke right away is very important. You have the best chance for full recovery if treatment to open a blocked artery is given within 4 hours of symptom onset. The sooner treatment occurs, the better your chances of recovery.
How Is Carotid Artery Disease Diagnosed?
Your doctor will diagnose carotid artery disease based on your medical history, a physical exam, and test results.
Medical History
Your doctor will find out whether you have any of the major risk factors for carotid artery disease. He or she also will ask whether you've had any signs or symptoms of a mini-stroke or stroke.
Physical Exam
To check your carotid arteries, your doctor will listen to them with a stethoscope. He or she will listen for a whooshing sound called a bruit. This sound may indicate changed or reduced blood flow due to plaque buildup. To find out more, your doctor may recommend tests.
Diagnostic Tests
The following tests are common for diagnosing carotid artery disease. If you have symptoms of a mini-stroke or stroke, your doctor may use other tests as well.
Carotid Ultrasound
Carotid ultrasound (also called sonography) is the most common test for diagnosing carotid artery disease. It's a painless, harmless test that uses sound waves to create pictures of the insides of your carotid arteries. This test can show whether plaque has narrowed your carotid arteries, and how narrow they are.
A standard carotid ultrasound shows the structure of your carotid arteries. A Doppler carotid ultrasound shows how blood moves through your carotid arteries.
Carotid Angiography
Carotid angiography (an-jee-OG-ra-fee) is a special type of x ray. This test may be used if the ultrasound results are unclear or don't give your doctor enough information.
For this test, your doctor will inject a substance (called contrast dye) into a vein, most often in your leg. The dye travels to your carotid arteries and highlights them on x-ray pictures.
Magnetic Resonance Angiography
Magnetic resonance angiography (MRA) uses a large magnet and radio waves to take pictures of your carotid arteries. Your doctor can see these pictures on a computer screen.
For this test, your doctor may give you contrast dye to highlight your carotid arteries on the pictures.
Computed Tomography Angiography
Computed tomography (to-MOG-rah-fee) angiography, or CT angiography, takes x-ray pictures of the body from many angles. A computer combines the pictures into two- and three-dimensional images.
For this test, your doctor may give you contrast dye to highlight your carotid arteries on the pictures.
How Is Carotid Artery Disease Treated?
Treatments for carotid artery disease may include healthy lifestyle changes, medicines, and medical procedures. The goals of treatment are to stop the disease from getting worse and to prevent a stroke. Your treatment will depend on your symptoms, how severe the disease is, and your age and overall health.
Heart-Healthy Lifestyle Changes
Your doctor may recommend heart-healthy lifestyle changes if you have carotid artery disease. Heart-healthy lifestyle changes include:
- Heart-healthy eating
- Maintaining a healthy weight
- Managing stress
- Physical activity
- Quitting smoking
Heart-Healthy Eating
Your doctor may recommend a heart-healthy eating plan, which should include:
- Fat-free or low-fat dairy products, such as skim milk
- Fish high in omega-3 fatty acids, such as salmon, tuna, and trout, about twice a week
- Fruits, such as apples, bananas, oranges, pears, and prunes
- Legumes, such as kidney beans, lentils, chickpeas, black-eyed peas, and lima beans
- Vegetables, such as broccoli, cabbage, and carrots
- Whole grains, such as oatmeal, brown rice, and corn tortillas
When following a heart-healthy diet, you should avoid eating:
- A lot of red meat
- Palm and coconut oils
- Sugary foods and beverages
Two nutrients in your diet make blood cholesterol levels rise:
- Saturated fat—found mostly in foods that come from animals
- Trans fat (trans fatty acids)—found in foods made with hydrogenated oils and fats, such as stick margarine; baked goods, such as cookies, cakes, and pies; crackers; frostings; and coffee creamers. Some trans fats also occur naturally in animal fats and meats.
Saturated fat raises your blood cholesterol more than anything else in your diet. When you follow a heart-healthy eating plan, only 5 percent to 6 percent of your daily calories should come from saturated fat. Food labels list the amounts of saturated fat. To help you stay on track, here are some examples:
|
If you eat: |
Try to eat no more than: |
|
1,200 calories a day |
8 grams of saturated fat a day |
|
1,500 calories a day |
10 grams of saturated fat a day |
|
1,800 calories a day |
12 grams of saturated fat a day |
|
2,000 calories a day |
13 grams of saturated fat a day |
|
2,500 calories a day |
17 grams of saturated fat a day |
Not all fats are bad. Monounsaturated and polyunsaturated fats actually help lower blood cholesterol levels.
Some sources of monounsaturated and polyunsaturated fats are:
- Avocados
- Corn, sunflower, and soybean oils
- Nuts and seeds, such as walnuts
- Olive, canola, peanut, safflower, and sesame oils
- Peanut butter
- Salmon and trout
- Tofu
Sodium
You should try to limit the amount of sodium that you eat. This means choosing and preparing foods that are lower in salt and sodium. Try to use low-sodium and “no added salt” foods and seasonings at the table or while cooking. Food labels tell you what you need to know about choosing foods that are lower in sodium. Try to eat no more than 2,300 milligrams of sodium a day. If you have high blood pressure, you may need to restrict your sodium intake even more.
Dietary Approaches to Stop Hypertension
Your doctor may recommend the Dietary Approaches to Stop Hypertension (DASH) eating plan if you have high blood pressure. The DASH eating plan focuses on fruits, vegetables, whole grains, and other foods that are heart healthy and low in fat, cholesterol, and sodium and salt.
The DASH eating plan is a good heart-healthy eating plan, even for those who don’t have high blood pressure. Read more about DASH.
Alcohol
Try to limit alcohol intake. Too much alcohol can raise your blood pressure and triglyceride levels, a type of fat found in the blood. Alcohol also adds extra calories, which may cause weight gain.
Men should have no more than two drinks containing alcohol a day. Women should have no more than one drink containing alcohol a day. One drink is:
- 12 ounces of beer
- 5 ounces of wine
- 1½ ounces of liquor
Maintaining a Healthy Weight
Maintaining a healthy weight is important for overall health and can lower your risk for carotid artery disease. Aim for a Healthy Weight by following a heart-healthy eating plan and keeping physically active.
Knowing your body mass index (BMI) helps you find out if you’re a healthy weight in relation to your height and gives an estimate of your total body fat. To figure out your BMI, check out the National Heart, Lung, and Blood Institute’s (NHLBI) online BMI calculator or talk to your doctor. A BMI:
- Below 18.5 is a sign that you are underweight.
- Between 18.5 and 24.9 is in the normal range.
- Between 25 and 29.9 is considered overweight.
- Of 30 or more is considered obese.
A general goal to aim for is a BMI of less than 25. Your doctor or health care provider can help you set an appropriate BMI goal.
Measuring waist circumference helps screen for possible health risks. If most of your fat is around your waist rather than at your hips, you’re at a higher risk for heart disease and type 2 diabetes. This risk may be high with a waist size that is greater than 35 inches for women or greater than 40 inches for men. To learn how to measure your waist, visit Assessing Your Weight and Health Risk.
If you’re overweight or obese, try to lose weight. A loss of just 3 percent to 5 percent of your current weight can lower your triglycerides, blood glucose, and the risk of developing type 2 diabetes. Greater amounts of weight loss can improve blood pressure readings, lower LDL cholesterol, and increase HDL cholesterol.
Managing Stress
Managing and coping with stress. Learning how to manage stress, relax, and cope with problems can improve your emotional and physical health. Consider healthy stress-reducing activities, such as:
- A stress management program
- Meditation
- Physical activity
- Relaxation therapy
- Talking things out with friends or family
Physical Activity
Routine physical activity can lower many risk factors for coronary heart disease, including LDL (“bad”) cholesterol, high blood pressure, and excess weight. Physical activity also can lower your risk for diabetes and raise your HDL cholesterol level. HDL is the “good” cholesterol that helps prevent coronary heart disease.
Everyone should try to participate in moderate-intensity aerobic exercise at least 2 hours and 30 minutes per week, or vigorous aerobic exercise for 1 hour and 15 minutes per week. Aerobic exercise, such as brisk walking, is any exercise in which your heart beats faster and you use more oxygen than usual. The more active you are, the more you will benefit. Participate in aerobic exercise for at least 10 minutes at a time spread throughout the week.
Read more about physical activity at:
- Physical Activity and Your Heart
- U.S. Department of Health and Human Services’ 2008 Physical Activity Guidelines for Americans
Talk with your doctor before you start a new exercise plan. Ask your doctor how much and what kinds of physical activity are safe for you.
Quitting Smoking
If you smoke, quit. Smoking can raise your risk for coronary heart disease and heart attack and worsen other coronary heart disease risk factors. Talk with your doctor about programs and products that can help you quit smoking. Also, try to avoid secondhand smoke.
If you have trouble quitting smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking.
Read more about quitting smoking at Smoking and Your Heart.
Medicines
If you have a stroke caused by a blood clot, you may be given a clot-dissolving, or clot-busting, medication. This type of medication must be given within 4 hours of symptom onset. The sooner treatment occurs, the better your chances of recovery. If you think you’re having a stroke, call 9–1–1 right away for emergency care.
Medicines to prevent blood clots are the mainstay treatment for people who have carotid artery disease. They prevent platelets from clumping together and forming blood clots in your carotid arteries, which can lead to a stroke. Two common medications are:
- Aspirin
- Clopidogrel
Sometimes lifestyle changes alone aren’t enough to control your cholesterol levels. For example, you also may need statin medications to control or lower your cholesterol. By lowering your blood cholesterol level, you can decrease your chance of having a heart attack or stroke. Doctors usually prescribe statins for people who have:
- Diabetes
- Heart disease or have had a stroke
- High LDL cholesterol levels
Doctors may discuss beginning statin treatment with those who have an elevated risk for developing heart disease or having a stroke.
You may need other medications to treat diseases and conditions that damage the carotid arteries. Your doctor also may prescribe medications to:
- Lower your blood pressure.
- Lower your blood sugar level.
- Prevent blood clots from forming, which can lead to stroke.
- Prevent or reduce inflammation.
Take all medicines regularly, as your doctor prescribes. Don’t change the amount of your medicine or skip a dose unless your doctor tells you to. Your health care team will help find a treatment plan that’s right for you.
Medical Procedures
You may need a medical procedure if you have symptoms caused by the narrowing of the carotid artery. Doctors use one of two methods to open narrowed or blocked carotid arteries: carotid endarterectomy and carotid artery angioplasty and stenting.
Carotid Endarterectomy
Carotid endarterectomy is mainly for people whose carotid arteries are blocked 50 percent or more.
For the procedure, a surgeon will make a cut in your neck to reach the narrowed or blocked carotid artery. Next, he or she will make a cut in the blocked part of the artery and remove the artery’s inner lining that is blocking the blood flow.
Finally, your surgeon will close the artery with stitches and stop any bleeding. He or she will then close the cut in your neck.
Carotid Endarterectomy
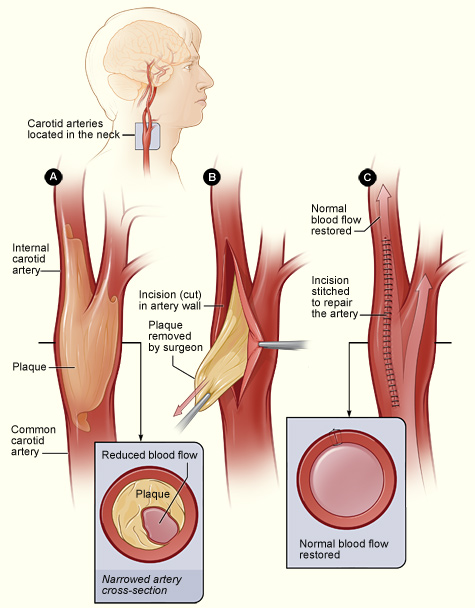
The illustration shows the process of carotid endarterectomy. Figure A shows a carotid artery with plaque buildup. The inset image shows a cross-section of the narrowed carotid artery. Figure B shows how the carotid artery is cut and how the plaque is removed. Figure C shows the artery stitched up and normal blood flow restored. The inset image shows a cross-section of the artery with plaque removed and normal blood flow restored.
Carotid Artery Angioplasty and Stenting
Doctors use a procedure called angioplasty to widen the carotid arteries and restore blood flow to the brain.
A thin tube with a deflated balloon on the end is threaded through a blood vessel in your neck to the narrowed or blocked carotid artery. Once in place, the balloon is inflated to push the plaque outward against the wall of the artery.
A stent (a small mesh tube) is then put in the artery to support the inner artery wall. The stent also helps prevent the artery from becoming narrowed or blocked again.
Carotid Artery Stenting
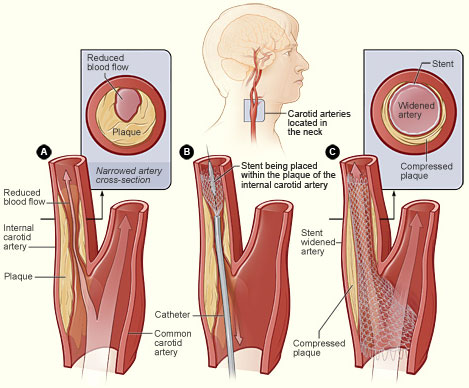
The illustration shows the process of carotid artery stenting. Figure A shows an internal carotid artery that has plaque buildup and reduced blood flow. The inset image shows a cross-section of the narrowed carotid artery. Figure B shows a stent being placed in the carotid artery to support the inner artery wall and keep the artery open. Figure C shows normal blood flow restored in the stent-widened artery. The inset image shows a cross-section of the stent-widened artery.
A stroke can also occur if blood clots form in the carotid arteries. This can happen if the plaque in an artery cracks or ruptures. Blood cell fragments called platelets (PLATE-lets) stick to the site of the injury and may clump together to form blood clots. Blood clots can partially, or fully, block a carotid artery.
A piece of plaque or a blood clot can also break away from the wall of the carotid artery. The plaque or clot can travel through the bloodstream and get stuck in one of the brain's smaller arteries. This can block blood flow in the artery and cause a stroke.
Carotid artery disease may not cause signs or symptoms until the carotid arteries are severely narrowed or blocked. For some people, a stroke is the first sign of the disease.
Outlook
Carotid artery disease is a major cause of stroke in the United States. Other conditions, such as certain heart problems and bleeding in the brain, can also cause strokes. Lifestyle changes, medicines, and medical procedures can help prevent or treat carotid artery disease and may reduce the risk of stroke.
If you think you're having a stroke, you need urgent treatment. Call 9–1–1 right away if you have symptoms of a stroke. Do not drive yourself to the hospital. You have the best chance for full recovery if treatment to open a blocked artery is given within 4 hours of symptom onset. The sooner treatment occurs, the better your chances of recovery.
How Can Atherosclerosis Be Prevented or Delayed?
Taking action to control your risk factors can help prevent or delay atherosclerosis and its related diseases. Your risk for atherosclerosis increases with the number of risk factors you have.
One step you can take is to adopt a healthy lifestyle, which can include:
Heart-Healthy Eating. Adopt heart-healthy eating habits, which include eating different fruits and vegetables (including beans and peas), whole grains, lean meats, poultry without skin, seafood, and fat-free or low-fat milk and dairy products. A heart-healthy diet is low in sodium, added sugar, solid fats, and refined grains. Following a heart-healthy diet is an important part of a healthy lifestyle.
Physical Activity. Be as physically active as you can. Physical activity can improve your fitness level and your health. Ask your doctor what types and amounts of activity are safe for you.
Quit Smoking. If you smoke, quit. Smoking can damage and tighten blood vessels and raise your risk for atherosclerosis. Talk with your doctor about programs and products that can help you quit. Also, try to avoid secondhand smoke.
Weight Control. If you’re overweight or obese, work with your doctor to create a reasonable weight-loss plan. Controlling your weight helps you control risk factors for atherosclerosis.
Other steps that can prevent or delay atherosclerosis include knowing your family history of atherosclerosis. If you or someone in your family has an atherosclerosis-related disease, be sure to tell your doctor.
If lifestyle changes aren’t enough, your doctor may prescribe medicines to control your atherosclerosis risk factors. Take all of your medicines as your doctor advises.
Living With Atherosclerosis
Improved treatments have reduced the number of deaths from atherosclerosis-related diseases. These treatments also have improved the quality of life for people who have these diseases.
Adopting a healthy lifestyle may help you prevent or delay atherosclerosis and the problems it can cause. This, along with ongoing medical care, can help you avoid the problems of atherosclerosis and live a long, healthy life.
Researchers continue to look for ways to improve the health of people who have atherosclerosis or may develop it.
Ongoing Care
If you have atherosclerosis, work closely with your doctor and other health care providers to avoid serious problems, such as heart attack and stroke.
Follow your treatment plan and take all of your medicines as your doctor prescribes. Your doctor will let you know how often you should schedule office visits or blood tests. Be sure to let your doctor know if you have new or worsening symptoms.
Emotional Issues and Support
Having an atherosclerosis-related disease may cause fear, anxiety, depression, and stress. Talk about how you feel with your doctor. Talking to a professional counselor can also help. If you're very depressed, your doctor may recommend medicines or other treatments that can improve your quality of life.
Community resources are available to help you learn more about atherosclerosis. Contact your local public health departments, hospitals, and local chapters of national health organizations to learn more about available resources in your area.
Talk about your lifestyle changes with your family and friends—whoever can provide support or needs to understand why you're changing your habits.
Family and friends may be able to help you make lifestyle changes. For example, they can help you plan healthier meals. Because atherosclerosis tends to run in families, your lifestyle changes may help your other family members too.
Links to Other Information About Atherosclerosis
NHLBI Resources
- Angina
- Carotid Artery Disease
- Coronary Heart Disease
- Coronary Heart Disease Risk Factors
- DASH Eating Plan
- Heart & Vascular Diseases
- Heart Attack
- Heart Disease in Women
- Peripheral Artery Disease
- Physical Activity and Your Heart
- Smoking and Your Heart
Non-NHLBI Resources
- Atherosclerosis (MedlinePlus)
- Carotid Artery Disease (MedlinePlus)
- Chronic Kidney Disease (National Institute of Diabetes and Digestive and Kidney Diseases)
- Coronary Artery Disease (MedlinePlus)
- Peripheral Arterial Disease (MedlinePlus)
™ Keep the Beat is a trademark of the U.S. Department of Health and Human Services.
